Urodynamics Testing
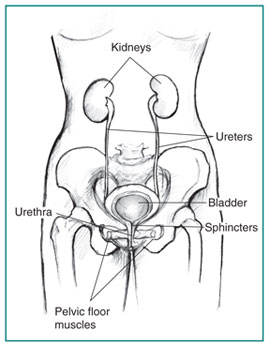
Urodynamics testing measures how well the bladder, sphincters, and urethra store and release urine. Most urodynamics testing focus on the bladder’s ability to hold urine and empty steadily and completely. These tests help diagnose patients who have lower urinary tract symptoms such as:
- urine leakage (incontinence)
- frequent urination
- painful urination
- sudden, strong urges to urinate (overactive bladder)
- problems starting a urine stream
- problems emptying the bladder completely
- recurrent urinary tract infections
Urodynamic Tests
Depending on your preliminary diagnosis, your doctor may recommend one or more of these urodynamic tests:
• uroflowmetry
• postvoid residual measurement
• cystometric test
• leak point pressure measurement
• pressure flow study
• electromyography
• video urodynamic tests
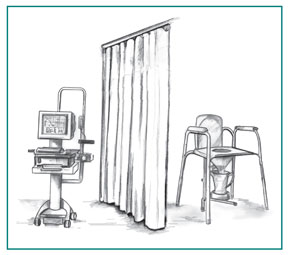
Uroflometry Testing Setup
Uroflowmetry
Uroflowmetry is the measurement of urine speed and volume. For this test, patients urinate privately into a special toilet or funnel that has a container for collecting the urine and a scale. The equipment creates a graph that shows changes in flow rate from second to second so the health care provider can see when the flow rate is the highest and how many seconds it takes to get there. Results of this test will be abnormal if the bladder muscles are weak or urine flow is blocked.
Postvoid Residual Measurement
This urodynamic test measures the amount of urine left in the bladder after urination. The remaining urine is called the postvoid residual. Postvoid residual can be measured with ultrasound equipment that uses harmless sound waves to create a picture of the bladder. Postvoid residual can also be measured using a catheter—a thin flexible tube inserted into the urethra.
Cystometric Test
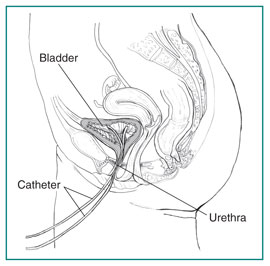
A cystometric test measures how much urine the bladder can hold, how much pressure builds up inside the bladder as itstores urine, and how full it is when the urge to urinate occurs. A catheter is used to empty the bladder completely. Then a special, smaller catheter is placed in the bladder. This catheter has a pressure-measuring device called a manometer. Another catheter may be placed in the rectum to record pressure there.
Once the bladder is emptied completely, the bladder is filled slowly with warm water. During this time, the person is asked to describe how the bladder feels and indicate when the need to urinate arises. When the urge to urinate occurs, the volume of water and the bladder pressure are recorded. The person may be asked to cough or strain during this procedure to see if the bladder pressure changes. A cystometric test can also identify involuntary bladder contractions.
Leak Point Pressure Measurement
This urodynamic test measures pressure at the point of leakage during a cystometric test. While the bladder is being filled for the cystometric test, it may suddenly contract and squeeze some water out without warning. The manometer measures the pressure inside the bladder when this leakage occurs. This reading may provide information about the kind of bladder problem that exists. The person may be asked to apply abdominal pressure to the bladder by coughing, shifting position, or trying to exhale while holding the nose and mouth. These actions help the health care provider evaluate the sphincters.
Pressure Flow Study
A pressure flow study measures the bladder pressure required to urinate and the flow rate a given pressure generates. After the cystometric test, the person empties the bladder, during which time a manometer is used to measure bladder pressure and flow rate. This pressure flow study helps identify bladder outlet blockage that men may experience with prostate enlargement. Bladder outlet blockage is less common in women but can occur with a cystocele or, rarely, after a surgical procedure for urinary incontinence.
Pressure Flow Study
Electromyography uses special sensors to measure the electrical activity of the muscles and nerves in and around the bladder and the sphincters.
Sensors are placed on the skin near the urethra and rectum or on a urethral or rectal catheter, and muscle and nerve activity are recorded. The patterns of the nerve impulses show whether the messages sent to the bladder and sphincters are coordinated correctly.
Video Urodynamic Tests
Video urodynamic tests take pictures and videos of the bladder during filling and emptying using X-ray (or fluoroscopy). The pictures and videos show the size and shape of the bladder and help the health care provider understand the possible problems.
Preparing for a Urodynamics Evaluation
- Do not consume any caffeine the day of the study
- Stop taking the following medications 3 days prior to testing unless otherwise instructed by your provider. (Continue taking all other prescription medications.)
AZO Standard
Detrol/ Detrol LA (tolterodine)
Enablex (darifenacin)
hyoscyamine, methenamine, methylene blue (Urimax, Urelle, Urised, Urisym, Utira, Prosed, UTA, Urogesic)
Myrbetriq (mirabegron)
oxybutynin/oxybutynin er (Ditropan, Ditropan XL, Oxytrol, Gelnique)
Pyridium (phenazopyridine)
Sanctura/Sanctura XL (trospium)
Urecholine (bethanechol)
Urispas (flavoxate)
Vesicare (solifenacin)
- If you are pregnant, please call the clinic right away. Your urodynamics evaluation may need to be postponed.
- If you have symptoms of burning or stinging with urination the day before the test, please call us, as your test may need to be postponed.
- If you have chronic constipation, use a Fleets enema (available over the counter) the day before your appointment.
- If your urologist gave you antibiotics, take them as prescribed. If they did not give you an antibiotic, the urodynamics staff will provide one.
- Eat a normal meal the day of the study, but remember no caffeine.
- Drink enough water so that you arrive at your appointment with a full bladder. (If you have a Foley catheter, there is no need to drink more water than normal.)
After Urodynamics Testing
After having urodynamic tests, a person may feel mild discomfort for a few hours when urinating. Drinking an 8-ounce glass of water every half-hour for 2 hours may help to reduce the discomfort. Taking a warm bath after the study may also help relieve any discomfort.
Urodynamics testing involves a small risk of developing a urinary tract infection or experiencing urinary frequency and/or urgency. You may also notice a small amount of blood in the urine. Should any of these symptoms continue for more than 24 hours after the testing, please call your provider for instructions.
An antibiotic may be prescribed for 1 or 2 days to prevent infection, but not always. People with signs of infection—including pain, chills, or fever—should call their healthcare provider immediately.
Results and Follow Up
Results of urodynamic testing can take 7-10 days to be forwarded to your provider because they are reviewed and interpreted by a professional.
